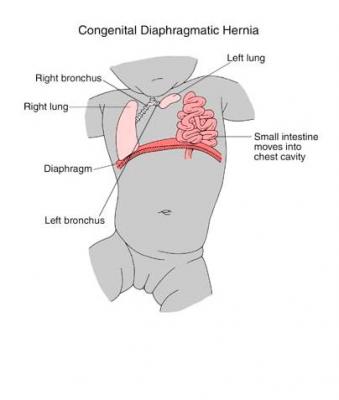
 Congenital diaphragmatic hernia is a congenital birth defect caused by either a hole in the diaphragm or the absence of the diaphragm. Due to the absence of, or hole in, the diaphragm the organs (may include the stomach, spleen, intestines, and liver) located in the abdomen move into the chest area. Those organs press again the lungs and prevent proper development of the lungs. Congenital diaphragmatic hernia is more common on the left side of the body. The cause of congenital diaphragmatic hernia is unknown.
Congenital diaphragmatic hernia is a congenital birth defect caused by either a hole in the diaphragm or the absence of the diaphragm. Due to the absence of, or hole in, the diaphragm the organs (may include the stomach, spleen, intestines, and liver) located in the abdomen move into the chest area. Those organs press again the lungs and prevent proper development of the lungs. Congenital diaphragmatic hernia is more common on the left side of the body. The cause of congenital diaphragmatic hernia is unknown.
Frequency
Congenital diaphragmatic hernia makes up approximately 8 percent of all major birth defects meaning it is seen in 1 in 3000 to 1 in 5000 live births per year.
Diagnosis
Congenital diaphragmatic hernia is detected by ultrasound during the second trimester. The physician may suspect congenial diaphragmatic hernia when the stomach is not in the typical location and the bowel is next to the heart. Please be aware that a right sided hernia is harder to detect.
Management Options and Outcomes
After detection, the physicians will perform several ultrasounds during the pregnancy to closely monitor the baby, determine the severity of the hernia and the check the amount of amniotic fluid. An important aspect of the monitoring will be the calculation of the lung-head ration (LHR). The LHR is a good predictor to determine the severity of damage to the lungs. If fetal surgery is not an option – after the baby is born the doctors will move the organs that have moved into the upper chest back into the abdomen in to their normal location.
Candidacy for Fetal Treatment
Yes at several centers around the country – one of the primary qualifications is a severe case of congenital diaphragmatic hernia. Otherwise corrective surgery will be done after birth.
Inclusion Criteria
- The following must be present before the doctor will perform a tracheal occlusion:
- Confirmed CDH with a portion of the liver herniated into chest
- Lung to head ratio less than or equal to 0.9 to 1.0
- Normal amniocentesis showing the absence of other major congenital anomalies
- Less than 26 weeks gestation
- Non-obese mother
Exclusion Criteria
If the following are present the doctor will not perform the tracheal occlusion:
- Abnormal amniocentesis
- Ruptured membranes
- Abnormal uterus
- Preterm uterus
- Other birth defects in the fetus
- BMI greater than 35
Details of Procedures
The doctor will provide a tracheal occlusion between weeks 26 to 29 followed by removal of the occlusion at 32 to 34 weeks gestation. A tracheal occlusion is when the doctors make a tiny incision in the mother and in the mother’s uterus and a tiny detachable balloon is placed in the fetal trachea. After surgery and until the balloon is removed you will have to have weekly ultrasounds. The balloon is removed after the lungs have developed. Both insertion and removal are done in utero.
Postoperative Care
The baby will unlikely be able to breathe on its own due to the underdevelopment to the lungs but that all depends on how severely the developing lungs were compromised due to the hernia.
Additional Information
Long term effects – up to 60% of infants with CDH will have gastroesophogeal reflux. Approximately 20 to 30% will experience some neurologic issues.
Additional Resources to Learn about CDH
- Video: FETO visually explained by Dr. Crombleholme of Connecticut Children’s.
- New Fetal Surgery Treatment for Congenital Diaphragmatic Hernia
- UCSF Fetal Treatment Center – Informative Videos
- CHERUBS – The Association of Congenital Diaphragmatic Hernia Research, Awareness and Support
- Home at Last: Parker Overcomes a Life-Threatening CDH Diagnosis
- Chase’s CDH Survivor Story
- Hugh’s Story of Hope
